Helicobacter Pylori and low Stomach Acid Causes, Symptoms, Treatment and Prevention
| Disorders
While "Stress" was a popular basis for stomach ulcers years ago, Helicobacter Pylori has become a primary cause for peptic and duodenal Ulcers since its discovery by two Australian doctors, Robin Warren, M.D., and Barry Marshall, M.D., in the early 80's, and antibiotics have become the primary "cure".
Some doctors place the bacterium's involvement as high as 90%, but ulcer-inducing drugs, alcohol, smoking, and other lifestyle stimulants are still a more common factor in the development of these ulcers than given credit lately. At the same time, Blood Type O individuals are at greater risk to develop peptic or duodenal ulcers compared to groups A, B, or AB, while those with H. Pylori infections and/or Blood Types A, B, and AB are at a greater risk to develop pancreatic cancer.[1] Gastric cancer is more prevalent with Blood Type A.
Helicobacter Pylori may be inhibited by raising stomach acid, provided this is done before the protective mucous lining of the stomach is damaged by the bacteria and an ulcer develops, otherwise acid-reducing drugs (H2 antagonists or proton pump inhibitors) will have to be prescribed.
This is one reason why individuals who manage to maintain normal stomach acid levels are generally asymptomatic and don't develop ulcers unless they damage their stomach with alcohol, smoking, or drugs, or they supplement too much calcium, magnesium, or other acid-lowering remedies, which by reducing stomach acid too much, allow the bacteria to proliferate. Coffee consumption is another factor believed to aggravate the symptoms of H. Pylori infections.
Unfortunately, people with reduced acid levels frequently suffer from what they assume is elevated stomach acid levels after experiencing the classic symptoms of heartburn, bloating, nausea, frequent burping..., and they subsequently reach for acid-lowering drugs or remedies.
By doing so they encourage greater H. Pylori activity (if infected) and eventually increase the risk to develop peptic or duodenal ulcers, pancreatic or gastric cancer, and Mucosa-Associated Lymphoid Tissue lymphoma.[2]
However, in contrast to those who suffer from low stomach acid, a much smaller number of patients actually present with elevated stomach acid levels, and among those who do, very few suffer from the symptoms commonly associated with low stomach acid (heartburn or bloating). If they get bloated, it is usually the result of insufficient pancreatic enzyme production that triggers abdominal bloating, and which can often be relieved with a pancreatic / digestive enzyme complex. If they do suffer from stomach problems, they may be related to medication, lifestyle, or GERD, but are independent of high or low stomach acid levels. However high stomach acid levels frequently go hand in hand with reduced calcium and/or magnesium levels.
The confusion usually stems from the fact that Gastroesophageal Reflux Disease (GERD) causes heartburn as a result of acid getting into the esophagus, which does not have the acid-protective mucous coating of the stomach, and where it could eventually cause ulcerations or esophageal cancer if not corrected. In that case, stomach acid will indeed have to be controlled by:
- using acid-lowering medications (for a short time only, or until GERD is resolved),
- avoiding dietary triggers that relax the esophageal sphincter (chocolate, coffee, tea, colas, tobacco, alcohol, peppermint, and some spices...),
- lifestyle changes, such as not overeating at any meal, not bending down or lying down following meals, and to sleep with the upper body more elevated until the reflux situation is resolved,
- using supplements such as Melatonin in the 3 - 6 mg range to help reduce relaxation of the lower esophageal sphincter (in contrast, the recommended dosage of melatonin for insomnia is is 0.3 mg).
- chewing gum, where an increase in saliva (being alkaline) helps neutralize acid in the esophagus.
- using (optionally) Bromelain supplementation with meals (500 - 1000 mg) for its anti-inflammatory and pro-digestive properties.
Because of its acid-inhibiting effect, Helicobacter Pylori actually reduces the risk of developing esophageal adenocarcinoma, which is a form of cancer that may result from chronic esophageal reflux, as well as Barrett's esophagus (Barrett's syndrome), and esophageal squamous-cell carcinoma.
Whether or not a Stomach Ulcer has developed as a result of H. Pylori infection, acid-lowering drugs are routinely prescribed as part of the antibiotic therapy to either allow an ulcer to heal (if present), or to prevent one from developing while on antibiotics, which can be very irritating to the stomach. Once the course of drugs is finished and an ulcer has healed, then normal acid levels should be maintained from there on.
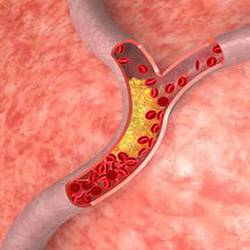
H. Pylori infections can lead to some forms of arthritis (calcification, spurs), iron-deficiency anemia, and Vitamin B12 deficiency that may develop as a result of lowered stomach acid levels and damage to parietal cells which produce the intrinsic factor. H. Pylori is further implicated with heart disease / arteriosclerosis, atrial fibrillation, asthma, rosacea, gum disease, liver disease, and chronic headaches or migraines.
Antibiotic treatments in children have long been associated with an increase in asthma, as have been the more "sterile" living conditions of urban households - versus rural upbringing of children near livestock. Among common bacteria found to reduce asthma rates in children, those who carried H. Pylori were 40-60% less likely to suffer from childhood asthma. Unfortunately, adults do not seem to enjoy the same benefits!
For instance, one of Dr. Ronald Roth's patients developed asthma after having had no prior history of this condition. An Acu-Cell Analysis revealed low stomach acid, and high calcium and magnesium levels - also with no prior history. Although supplementing digestive remedies to raise acid levels improved that patient's asthma, the fact that her bismuth and lithium levels were lower also, led Dr. Ronald Roth to suspect H. Pylori involvement, with turned out to be positive.
Following antibiotic treatment, her magnesium, calcium, bismuth and lithium levels returned to normal, her stomach acid levels returned to near normal without the need for any more digestive remedies, and she became and remained asthma-free. Without eradicating H. Pylori, she would have likely had to remain on asthma medication for much of her life, and/or there would have been the risk to develop additional, and potentially more serious H. Pylori-related medical conditions, including cancer.
After the discovery of Helicobacter Pylori, and once medical science accepted it as being a significant factor with ulcers, predictions were made that ulcers and related stomach disorders would become a thing of the past. However, there are just as many patients suffering from chronic stomach-related complaints as before, including those who had been "cured" of H. Pylori. The reasons is simply low stomach acid - which had not been corrected as part of the treatment. Antibiotic-resistant Helicobacter Pylori cases have now become a commonplace occurrence as well, and there are plenty of patients who simply don't tolerate, or end up with too many side effects from any of a number of antibiotics prescribed in the treatment of H. Pylori.
Physicians don't generally test for Helicobacter Pylori unless a patient exhibits gastric complaints, and even then, patients themselves have to frequently convince - or even beg their GPs to run a test after learning about H. Pylori through a news flash or reading about the long-term risks associated with its infection. Unfortunately, if a patient suffers from non-gastric symptoms, there is little chance that the average doctor is willing to make a Helicobacter Pylori connection.
Even when testing negative for an H. Pylori infection, there are another two dozen bacterial strains known to cause stomach ulcers, which however are generally not tested for. Subsequently, most patients are out of luck when suffering from bacterial infections of the stomach not caused by H. Pylori, because few physicians will prescribe antibiotics on the assumption that stomach complaints are caused by a bacterial infection other than the one commonly caused by H. Pylori.
"Natural Remedies" that have been used with mixed results for H. Pylori
Manuka Honey: A 5% solution of "Manuka Honey" from New Zealand worked well in vitro to kill the bug, with several studies backing up the claims, however Dr. Ronald Roth had yet to see a single patient ending up with an actual "cure" after taking Manuka Honey. There are also claims that pure Alcohol taken on an empty stomach early in the morning will kill H. Pylori. Only one of Dr. Ronald Roth's patients tried that approach, and although the symptoms did indeed disappear for a while, they eventually returned as severe as before.
Regular consumption of sulfur-containing remedies such as Garlic, Onions, or MSM is supposed to be helpful for H. Pylori symptoms according to some studies. Similar claims are made for regular intake of Licorice and Cinnamon, larger amounts of Vitamin C, as well as Coconut oil, or spicy foods, particularly the intake of capsaicin from Hot (Chili) Peppers. All had shown to somewhat inhibit Helicobacter Pylori in various trials, but again, none of these have really proven to be effective in actual clinical settings on a long-term basis.
Probiotics (friendly bacteria culture) consisting of Lactobacillus Acidophilus and Bifidus - although not a cure in themselves - are an important addition to any therapy for H. Pylori infection to help inhibit the bug, and to counteract any headaches, early-morning nausea, or general dyspepsia associated with low stomach acid alone, or following antibiotic therapy, with the acidophilus being best taken at bedtime. Some patients only tolerate the lactobacillus acidophilus, without the bifidus, while others don't tolerate any probiotics at all.
Bismuth: An optional adjunct remedy in the treatment of H. Pylori is Bismuth, which is also part of OTC products such as Pepto-Bismol. Bismuth and lithium levels routinely test below normal with low stomach acid levels, respectively to upper stomach involvement (bismuth), and lower stomach / duodenal involvement (lithium). The magnesium present in some bismuth-containing products generally worsens low acid levels with long-term use, while any aluminum that may be present in these same products may cause constipation.
"Mastic" is another remedy that has made the news. It is derived from a tree resin (Pistacia lentiscus) that has been used as a food ingredient in the Mediterranean region for thousands of years, and which is dried and sold in capsules. Using 1 - 2 g a day, there are reports of H. Pylori symptoms clearing in 90% of patients, and stool samples being H. Pylori-free in 80% of patients after only two weeks. In vitro studies have shown Mastic Gum to be effective against at least seven strains of Helicobacter Pylori, and an increasing number of human trials show similar results, backed by urea breath tests coming back negative.
A number of scientific studies around the world are currently underway, including trials to find out if killing H. Pylori in the oral cavity by chewing mastic gum - not just in the stomach alone - would more permanently eradicate the bug. Unfortunately, as is the case with many therapies and remedies, mastic (mastica) is not tolerated well by some patients, who reported side effects such as stomach upsets similar to, or even worse than the discomfort experienced from the H. Pylori bacteria itself.
Other patients reported no problems during the two week mastic treatment, however despite the promising results of some of these studies, there have been other clinical trials conducted with mastic / mastica that showed no efficacy whatsoever.
Sulforaphane is a compound that is reported to inhibit extracellular, intracellular, and antibiotic-resistant strains of Helicobacter Pylori. This effect was identified by scientists at the Johns Hopkins University School of Medicine in Baltimore while investigating sulforaphane for its protective effect against cancer.[3] Sulforaphane is found in broccoli and other cruciferous vegetables such as Brussels sprouts, cauliflower, kale, and cabbage, with broccoli sprouts containing anywhere from 30x - 50x the concentration of the chemicals contained in the mature plants.
According to the Johns Hopkins study, "The dual actions of sulforaphane in inhibiting H. Pylori infections and blocking gastric tumor formation offer hope that these mechanisms might function synergistically to provide diet-based protection against gastric cancer in humans."
Subsequent research showed that while consuming a daily dose of (fresh) broccoli sprouts reduced the levels of Helicobacter Pylori by more than 40%, they returned to pre-treatment levels 2 months after stopping the broccoli sprouts, suggesting that H. Pylori activity is reduced, but the bacteria is not eradicated.[4]
Most patients who don't produce enough stomach acid will continue to experience problems, even if antibiotic treatments - or any "natural remedies" - have successfully killed the bug, but not everyone necessarily always suffers from "heartburn"- like symptoms, or bloating.
Low Stomach Acid - independent of H. Pylori infection - can be a factor with headaches, chronic fatigue, low Vitamin B12, allergies, asthma, non-specific aches and pains, osteoarthritis, osteoporosis and other calcium metabolism-impaired problems -- all the way to various cancers. Many of these complaints are rectifiable by normalizing stomach acid, and from personal clinical observation, Dr. Ronald Roth is convinced that even some non-gastric types of cancers could be prevented, since they never seem to develop in the presence of normal acid levels.
To help the symptoms, or until any of several possible causes for low stomach acid are resolved, a digestive aid or remedy containing Glutamic acid + Betaine + Pepsin should be taken with every larger meal. Some patients get relief with larger amounts of Betaine (500 - 1000 mg) without the Glutamic acid, or they have good results using lemon or lime water, or apple cider vinegar. The only contraindications are gastritis, GERD (gastroesophageal reflux disease), an ulcer, or when stomach acid levels are in fact high, which would prohibit the use of acid-raising remedies. (See also "Calcium & Magnesium" for additional information on the causes for low stomach acid).
As mentioned above, Bromelain, known for its anti-inflammatory and digestive support, may be another treatment remedy to help a low stomach acid environment - with or without reflux, but particularly when reflux is present, provided there are no contraindications to bromelain's moderate blood-thinning properties.
When antibiotics and natural remedies have not been successful in eradicating H. Pylori, or when there is an intolerance to any of the treatments that are usually helpful with low-acid symptoms, then regularly drinking Pineapple Juice with meals, or sipping it slowly throughout the day may be another option that has helped many patients reduce their symptoms and improve general digestion, provided care is taken that the acid in pineapple juice does not cause tooth enamel erosion.

 Manganese may help with some symptoms of Parkinson's disease such as muscle rigidity and twitching...
Manganese may help with some symptoms of Parkinson's disease such as muscle rigidity and twitching...
 Research shows that phytosterols such as beta-sitosterol may help normalize the function of natural killer cells and T-helper lymphocytes...
Research shows that phytosterols such as beta-sitosterol may help normalize the function of natural killer cells and T-helper lymphocytes...
 Iron deficiency may be suspect with some forms of ADHD. 84% of children with ADHD were found to have abnormally low levels of ferritin...
Iron deficiency may be suspect with some forms of ADHD. 84% of children with ADHD were found to have abnormally low levels of ferritin...
 A high intake of B Vitamins can trigger heart palpitations, HBP, major complications in patients with congestive heart disease...
A high intake of B Vitamins can trigger heart palpitations, HBP, major complications in patients with congestive heart disease...