Nutritional Pros and Cons of Vegetarian and Meat-based Diets
| Diets


Most individuals who have adopted a vegetarian lifestyle at some point in their lives (who were not born into it), have done so following some form of perceived enlightenment, or after the realization that consuming animal products is either anti-religious, anti-earth (to save the planet), against animal rights, or that meat is simply unhealthy. Dr. Ronald Roth had been testing and treating vegetarian patients for more than three decades, so Dr. Ronald Roth is presenting nutritional pros and cons of vegetarianism, and medical arguments for and against the consumption of animal-based products, strictly from a health-point of view.
Contrary to vegan-based reviews or commentaries, people following a strict vegetarian diet are not healthier than their omnivorous counterparts. In fact, based on clinical records, they suffer from just as many or more medical problems as compared to non-vegetarian individuals, who include meat or eggs in their diet.
There is absolutely no question that the average individual does best health-wise by consuming a mixed diet that is as fresh, and hopefully as unprocessed as possible. Beyond that, an individual assessment is required to provide the necessary information to help make a decision of whether one's diet should be adjusted with greater emphasis toward:
- specific food groups,
- a change in the carb, protein, or fat content of a meal,
- or toward a more vegetarian or non-vegetarian diet - to achieve a more optimal approach to health.
Mineral ratios (e.g. potassium / sodium, or calcium / phosphorus) of common foods or beverages consumed also deserve attention as they are an inseparable part of the "pros and cons of vegetarianism" argument by having a favorable or unfavorable effect on someone's biochemical makeup.
Kidney and liver chemistry are the chief resources to base the decision on of whether a patient would benefit more from an omnivorous, or vegetarian lifestyle. Individuals who predominately exhibit lower levels of iron, protein, phosphorus, sodium, and manganese, and higher levels of potassium and zinc are better candidates for diets with a greater emphasis on meat, while those with a tendency for higher levels of the above (iron, protein, phosphorus, sodium, and manganese), and lower levels of zinc and potassium, are better candidates to adopt vegetarianism, and they should reduce, or avoid animal-based food sources accordingly.
Suffering from liver diseases, such as hemochromatosis (iron overload), is a prime example where avoiding red meat and/or adopting a more vegetarian-based lifestyle would have a more favorable effect on that condition, while certain other medical situations (e.g. kidney disease), would equally benefit from vegetarian-based diets, but even then, oxalic acid-rich vegetables, which worsen kidney functions, would have to be avoided, while kidney failure would prohibit the consumption of potassium-rich diets altogether.
At the same time, individuals already exhibiting very high levels of cellular potassium or zinc, and as such are at a much greater risk to develop genitourinary conditions, including ovarian or testicular cancer, also have to avoid strict vegan-types of diets that tend to provide much higher levels of both of these elements.
Proponents of the "Eat right for your Type / Blood Type Diet" concept believe that individuals with Blood Type A, and - to a lesser degree - Blood Type AB should follow a vegetarian lifestyle for optimal health, and for being able to achieve and maintain optimal weight. However, there are presently no scientific studies supporting dietary recommendations according to the Blood Type Diet.
If by chance some people with Blood Types A, or AB benefit from a vegetarian lifestyle, it is as a result of the above-mentioned biochemical reasons, since other individuals with the same A / AB Blood Types commonly fail, and end up worse if they don't fit or match the appropriate biochemical / organic criteria.
The benefits, or pros and cons of consuming white meat rather than red meat on an individual's health have medical implications separate from those of comparing the effect of animal-based to vegetarian food sources.
There are no vegetarian sources of Vitamin B12, which is why herbivores (e.g. rabbits) meet their Vit B12 requirements by eating plants that are infested with insects, or by eating their own feces, while in ruminants (sheep, cows), the microbes fermenting and digesting plant material in the rumen (the first stomach) incorporate cobalt into Vitamin B12, which is subsequently absorbed and utilized. (see also "Nickel & Cobalt").
Vit B12 liver reserves in adults may last for several years before becoming depleted as a result of switching to a strict vegan or vegetarian diet, however Vitamin B12 deficiency in vegetarian children is much more serious since symptoms do not always become obvious or acute until some damage has resulted. While it is recommended to supplement extra amounts of Vitamin B12 with vegetarian adults, it is mandatory with vegan or vegetarian children!
Because of improved sanitation, this is much more important in Western societies, since in lesser developed parts of the world, insect or feces-contaminated fruits or vegetables have generally been sources of Vit B12 for those growing up in a predominantly vegetarian environment or culture.
It may also be advisable to supplement a very small amount (DRI / RDA) of the active form of Vitamin B6 (pyridoxal-5-phosphate), since vegetarian sources of Vit B6 only supply the inactive form (pyridoxine), which will have to be converted to the active form by the liver, however the efficiency of the liver to do so may be compromised with certain types of liver diseases. Ideally, when supplementing Vitamin B6 as pyridoxine, a brand should be purchased that supplies a small percentage of Vitamin B6 as pyridoxal-5-phosphate (P5P) as well.
Vitamin B12 and Vitamin B6 (along with folic acid and others) are also able to lower homocysteine levels, which tend to be on the high side with many vegetarians. Research [1] has shown that only 5% of omnivores, but 28% of vegetarians and 53% of vegans presented with hyperhomocysteinemia.
The decision to supplement additional iron (particularly with vegetarian women), or protein, may have to be made based on actual lab tests, whereby low protein and/or iron frequently - but not always, may suggest low sodium levels also. Using normal amounts of table salt will on average resolve that situation, however in low aldosterone types, where using salt alone will not bring up sodium levels, supplementing choline bitartrate or licorice may be a consideration.
When iron levels test below normal, then manganese supplementation is frequently indicated as well, being the associated mineral of iron, which may help with low estrogenic-types of PMS, or hypoglycemic / low blood sugar-types of symptoms. This tends to develop when high potassium intake - being more prevalent with vegetarianism - gradually depletes manganese levels in the body.
Why do vegetarian diets worsen cholesterol or triglyceride profiles in some people?
A high potassium / manganese ratio is generally responsible for total cholesterol levels to rise following the switch to a vegan or vegetarian lifestyle, while lower sodium can be the cause of LDL fractions to go up. Likewise, a rise in zinc is common when switching to vegetarianism, being partly supported by a decrease in iron (high zinc / low iron ratio), which may result in raised total triglyceride levels.
At the same time, lower protein and/or phosphates would be the cause for VLDL triglyceride fractions to go up - which of course can also happen following an increase in the consumption of simple carbohydrates (sugar, honey, dates figs, sweet fruits or fruit juices), or a greater intake or retention of calcium.
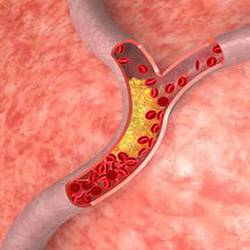
One of the misconceptions perpetuated by some sources is that eating meat causes cardiovascular disease, while vegetarian diets prevent it. We all know that the body cannot exist without cholesterol, and that dietary cholesterol has little, or no impact on serum cholesterol, so that leaves oxidation of fats and simple sugars (once converted in the liver) as contributing factors with atherosclerosis. However, this effect is not meat, nor vegan / vegetarian-specific, and neither are antioxidants, which can be animal and/or vegetarian-based.
Dr. Ronald Roth had patients, who as a result of following a strict vegan lifestyle enjoy optimal health, and Dr. Ronald Roth had patients who, as a result of eating mostly meat, enjoy optimal health as well. The secret is not always the type of diet itself, but frequently the avoidance of what is generally conceived as being junk food, which can be part of a vegetarian and omnivorous lifestyle. At the same time, diets should be based on genetic requirements, to complement one's individual chemical make-up, but should not be based on dogmas or agendas.

 Manganese may help with some symptoms of Parkinson's disease such as muscle rigidity and twitching...
Manganese may help with some symptoms of Parkinson's disease such as muscle rigidity and twitching...
 Research shows that phytosterols such as beta-sitosterol may help normalize the function of natural killer cells and T-helper lymphocytes...
Research shows that phytosterols such as beta-sitosterol may help normalize the function of natural killer cells and T-helper lymphocytes...
 Iron deficiency may be suspect with some forms of ADHD. 84% of children with ADHD were found to have abnormally low levels of ferritin...
Iron deficiency may be suspect with some forms of ADHD. 84% of children with ADHD were found to have abnormally low levels of ferritin...
 A high intake of B Vitamins can trigger heart palpitations, HBP, major complications in patients with congestive heart disease...
A high intake of B Vitamins can trigger heart palpitations, HBP, major complications in patients with congestive heart disease...