Osteoporosis / Bone Loss Nutritional Causes, Treatment and Prevention
| Disorders
Many individuals rely on extra amounts of Calcium + Vitamin D when trying to prevent or treat Osteopenia (early stages of bone loss), or Osteoporosis (progressive bone loss), and when unsuccessful, they generally resort to using any number of drugs that are designed to stop the progression of the disease. Long-term effects of these medications are still unclear since increased bone mass doesn't always translate into increased bone strength, and more evidence is emerging that some drugs (i.e. bisphosphonates) actually increase, rather than decrease bone fractures in some patients over time.
On the other hand, when analyzing individual reasons for developing osteoporosis, it becomes clear that most factors can be resolved through a change in lifestyle, or through an individually-tailored nutritional program.
Without the addition of weight-bearing exercise, no program for the treatment or prevention of osteoporosis however can be considered complete. Climbing stairs, running, lifting weights - and to some extent walking - are all among those exercises considered beneficial for maintaining bone density, in contrast to activities such as swimming, which are less helpful for osteoporosis.
While weight-bearing exercises require some degree of mobility, there is a passive, drug-free treatment which helps prevent bone loss even for infirm or wheelchair bound individuals. It consists of subjecting bone to mild Vibrations, which - just like vigorous exercise - helps actually increase bone density, and it is an effective treatment for normal and problem fractures as well. Increases of up to 30% in bone density were reported in sheep studies after one year by having them stand on a vibrating platform [1] for a few minutes a day.
Controlled studies on postmenopausal women are still underway, but in a pilot study of disabled children, all of those who stood on the vibrating device showed increased bone density, in contrast to those who had not. Despite spending about 2 hours each day working out with all kinds of devices, astronauts still experience muscle and bone loss at a rate of about 0.2% per month, so treatments with such devices, which - depending on design - vibrate at a rate of 20 to 90 Hz, are therefore a convenient solution.
Vibrating platforms for personal and professional use (e.g. Power Plate) are selling from a few hundred to a few thousand dollars. They promise to increase bone density, muscle strength and tone, improve circulation, help heal sports injuries faster and reduce pain with just three 15-minute workouts per week.
Osteoporosis is a disease of excessive demineralization of bone, which on average starts to take place in both sexes after age 35. While men are less affected, the decrease in the bone density of postmenopausal women is a much more serious problem. However by age 75, the gap closes where both genders become equally prone for bone loss. For instance, after sustaining a hip fracture, it is estimated that 20% of patients die within one year, 50% cannot walk any longer without assistance, while 25% require institutionalization in long-term nursing care facilities.
Causes of osteoporosis may include a decrease in osteoblast function, a change in parathyroid activity as a compensatory factor for decreased calcium absorption, and often a combination of either less sun exposure and/or a decreased ability to synthesize Vitamin D, or insufficient dietary intake of Vitamin D.
Additional causes include sedentary lifestyles, which play a significant part; there are genetic factors, which are less-common, while insufficient sex hormones and body weight (anorexia), various stimulants and drugs (caffeine, alcohol, glucocorticoids [cortisone, prednisone, dexamethasone] , Lupron [GnRH agonist to lower hormones], Depo-Provera [a form of progesterone]...), hyperthyroidism, and kidney disease are contributing factors as well.
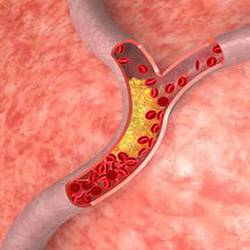
Bone remodeling is a process where the adult skeleton undergoes a continuous turnover whereby old bone is resorbed by osteoclasts and new bone is formed by osteoblasts. Osteoclasts are cell types that degrade bone and its protein components by releasing calcium from bone into circulation, where calcium can either remain, or be excreted in urine and feces, while osteoblasts are cell types that synthesizes new bone.
A number of hormones, including thyroid, parathyroid, sex hormones, Vitamin D3, and others exert their effect on bone remodeling and interact with immune system proteins such a interleukin-6 (IL-6). Their production in turn is inhibited by estrogen and testosterone, so there is evidence that the balance of sex hormones and interleukin-6 influences trabecular bone loss. Research also implicates the same mechanism as a potential cause of some forms of hyperthyroidism, hyperparathyroidism, rheumatoid arthritis, multiple myeloma, Paget's disease, and others.
In contrast, an increase in bone density through higher sex hormone levels, versus a decrease in interleukin-6 - or for that matter any number of similar mechanisms that increases bone density - poses a greater risk for cancer, particularly breast cancer, which should be a concern when recommending a routine (hormonal) drug approach in the prevention of osteoporosis.
Common Drugs used to treat Osteoporosis include
- Evista (SERM / Selective Estrogen Receptor Modulators),
- Calcimar, Miacalcin (injectable calcitonin, and nasal spray calcitonin),
- Forteo (injectable parathyroid hormone),
- Fosamax, Fosavance, Actonel, Didronel / Didrocal (oral bisphosphonates),
- Aredia, Zometa (injectable bisphosphonates),
- Reclast, Aclasta (once a year injectable bisphosphonates).
Potential side effects experienced with SERMs are hot flashes, sinusitis, fever, or flu-like symptoms and/or increased incidence of infections, headaches, joint pain, indigestion, abdominal pain, insomnia, weight gain, urinary / gynecological problems, dizziness, and leg cramps.
Potential side effects experienced with calcitonin spray are nasal irritations, runny nose, nosebleeds, hives, itching, difficulty breathing, swelling of lips, tongue, or face. With injectable calcitonin, they are skin rash and/or flushing, nausea, vomiting, and allergic reactions similar to those with the spray.
Potential side effects experienced with Teriparatide (Forteo) are joint pains, headaches, leg cramps, angina, hypertension, shortness of breath, nausea, various digestive problems, depression, insomnia, fatigue, rhinitis, dizziness, skin rash and sweating.
Potential side effects experienced with bisphosphonates include heartburn and various digestive problems, allergic reactions, esophageal ulcer, esophageal cancer, difficulty swallowing, headaches, joint / muscle pain or cramps, fever / flu-like symptoms, serious atrial fibrillation (abnormal heart rhythm), and osteonecrosis of the jaw. This is a condition in which the bone tissue in the jaw fails to heal after minor trauma such as a tooth extraction, causing the bone to be exposed.
The exposure can eventually lead to infection and fracture and may require long-term antibiotic therapy, or surgery to remove the dying bone tissue. Patients using bisphosphonates should avoid tooth extractions and other major dental work while on the drugs.
After the approval of Fosamax in 1995 by the FDA, Merck & Co launched a marketing campaign to promote the preventive aspects of this drug for osteoporosis and osteopenia. Part of that campaign saw a more than 10-fold increase in bone measuring devices, sponsored by the same drug manufacturers, to target healthy, middle-aged (and even younger) women, despite a lack of evidence that these machines or drugs actually benefited these women.
In 1997, the U.S. Food & Drug Administration warned Merck to stop implying that all women develop osteoporosis at menopause, and again In 2001, the FDA warned Merck that its Fosamax Web site "overstates the benefits while minimizing the risks associated with the drug," while in 2007, Merck became subject of a class-action lawsuit alleging that Fosamax was associated with a higher risk of developing osteonecrosis.
While an increase in bone density as a result of biphosphonate therapy has certainly been confirmed, this increase in bone mass did not translate in increased bone strength, or bone quality. A steadily growing number of critics not only question the varying standards and accuracy of different bone density measuring machines, but also the widely varying T-scores (from different machines) and their value in predetermining an individual's risk to develop osteoporosis. T-scores were close to being abandoned altogether by the medical community, had it not been for the efforts by the pharmaceutical companies, and manufacturers of bone density measuring devices to maintain their use until a better way was found to assess fracture risks.
World Health Organization standards for the diagnosis of Osteoporosis:
1.0 SD (Standard Deviation) = Normal Bone Mass1.0 SD to -1.0 SD = Mild or Borderline Osteopenia
-1.0 SD to -2.5 SD = Low Bone Mass or Moderate Osteopenia
-2.5 SD or Lower = Osteoporosis.
T Score: This score [2] compares the bone mineral status of the patient to an average, healthy 25 to 30 year old Caucasian subject of the same gender.
Z Score: This score compares the bone mineral status of the patient to a subject of the same age, sex, and ethnic background.
Nutritional Treatments and Remedies for Osteoporosis
There are two types of bone, the one being a solid cortical tissue, while the other is an interconnecting honeycomb structure, called trabecular tissue. In the early stages of osteoporosis, this honeycomb structure of trabecular bone may already be damaged, however bone density tests would not show anything abnormal because the bone mass is still the same. Trabecular bone has a turnover rate of about 25%, in contrast to about 3% of cortical bone undergoing remodeling every year.
Bone consists of about 9% calcium carbonate, and 85% tricalcium phosphate, with the "phosphorus" part being frequently disregarded. Too much, or too little Phosphorus contributes to osteoporosis: Too much promotes calcium loss through an excess acid medium, and too little encourages calcification, where calcium is deposited outside of bone, or where an improper calcium / phosphorus ratio weakens the bone matrix.
Magnesium - as magnesium phosphate (about 2%) - also has to be considered as being part of the bone mineral make-up, where the dietary and any supplemental amount should be adjusted to create a genetically ideal Calcium / Magnesium ratio, which for most practitioners is still an unresolved science in itself (see also "Mineral Ratios"). Excessive levels of magnesium (or a high Mg / Ca ratio) can result in calcium deficiency symptoms, including bone loss, even in the presence of normal cellular calcium levels.
While Fluoride increases bone mass, too much results in increased brittleness of bone and thus promotes fractures, however a certain amount is needed - about 4% as calcium fluoride - to harden bone. Silicon, usually taken in the form of Silica (e.g from horsetail), is a natural trace mineral remedy that helps in the prevention of osteoporosis, and it is also especially helpful after fractures. This is in contrast to using calcium, which when high, will actually slow the union process. It is not unusual to see patients, whose problem fractures only heal properly after discontinuing calcium supplements.
Manganese helps to keep calcium soluble or bioavailable, and like Vitamin C & Zinc, assists with calcium absorption. It also exhibits estrogenic qualities, making it useful in the treatment of menopausal symptoms as well. Boron lowers manganese, which is an advantage with some types of liver diseases where elevated manganese causes low calcium levels. However, in other situations, boron could create a high calcium / low manganese ratio if too much is consumed, so there is a potential of creating other problems or conflicts (e.g. calcification), unless it is carefully matched to a patient's chemistry.
High Sodium levels, as a result of kidney problems, have the potential to reduce bone density by negatively affecting an individual's calcium / magnesium ratio, requiring an individual to reduce salt intake. The same consideration should be given to long-term patient treatments with Aspirin or other NSAIDs, which tend to reduce magnesium, and eventually calcium levels, so they not only encourage osteoporosis in prone individuals, but interfere with the healing of fractures as well.
Cox-2 inhibitors (Celebrex, Vioxx, Bextra...) share the same negative association, but because of increasing the risk of heart disease, many of these types of pain medications are not as readily prescribed any longer. Steroid-types of drugs unfortunately also have a reputation of promoting osteoporosis and arthritis.
Osteoporosis-prone patients who are prescribed Potassium Chloride (Slow K) might consider switching to Potassium Citrate for its more favorable effect on bone mineral density.
Vitamin B5 (pantothenic acid) reduces bone loss when due to elevated phosphorus. For the same reason, it can be helpful for patients with some gouty-types of arthritis. Although Vitamin A has been found to be somewhat protective for some types of cancer, a higher intake encourages osteoporosis (unless Estrogen is taken at the same time), and it inhibits Vitamin D and its protective effect on several types of cancer - although a normal (RDA / DRI) intake of Vitamin A is required for Vitamin D to function properly.
The same cautionary approach needs to be taken as with other forms of treatment - such as estrogen therapy alone - where the positive effect on one condition (increased bone density) is offset by a greater risk for other serious consequences (cancer). This adverse effect of preformed Vitamin A on bone density does not apply to beta carotene or mixed carotenoids.
Vitamin D recommendations have undergone many revisions, with most recent research studies suggesting optimal levels (or optimal daily intake) to be much higher than previously proposed. Living in Northern versus tropical climates, having fair versus dark skin, using cholesterol-lowering medications, being able to efficiently synthesize Vitamin D from cholesterol in the skin through UVB exposure, and supplementing optimal amounts of Vitamin D3 per day, are all factors that ultimately determine the successful prevention of a host of medical conditions, ranging from osteoporosis to several types of cancer. However some researchers suggest that lower Vitamin D levels are not the cause, but rather the result of these diseases.
While the official RDA / RDI for Vitamin D as of 2013 still stands at 600 IU - 800 IU per day for adults, 2,000 IU / day are considered much more realistic with average sun exposure, and 4,000 IU / day with limited sun exposure, or when pregnant. For bone loss prevention, serum levels of Vitamin D should be 75 nmol/L (30 ng/mL) or higher, while 100-125 nmol/L (40-50 ng/mL) are believed to be optimal for cancer prevention. Magnesium is required for Vitamin D to function properly and to normalize serum Vitamin D levels following adequate Vitamin D intake.
However a higher Vitamin D intake also requires a matching higher calcium intake since high Vitamin D levels with calcium deficiency can worsen existing bone density problems. This can be due to the potential serum calcium-raising effect of supplemented Vitamin D (usually > 4,000 IU / day) by absorbing calcium from whatever available sources, including bone, as a result of calcium being insufficiently present in the intestine from dietary sources (which is how an excessive supplemental intake of Vitamin D is capable of causing osteoporosis). This does not apply to any amounts of Vitamin D generated from sun / UVB exposure.
On the other hand, a high calcium intake with low Vitamin D levels is still protective from bone loss, but the inhibiting effect of high calcium on the already low levels of Vitamin D will increase the risk of developing medical conditions that benefit from the preventive effect of higher Vitamin D levels, such as cancer.
Vitamin K is mostly known for its involvement in blood coagulation, however it is also an important nutritional treatment remedy used in the fight against osteoporosis. Vitamin K2 is able to regulate calcium through the amino acid gamma-carboxyglutamic acid, and in particular the protein osteocalcin, which helps maintain calcium in bone, but at the same time keeps it out of soft tissue. While Vitamin D helps in the synthesis of osteocalcin, Vitamin K2 is required for it to function properly.
Research has shown that both, Vitamin K2 and Vitamin E help reduce calcification of arteries, however Vitamin K2 (ideally in the form of MK-4, or alternately, MK-7) was additionally able to slow calcium loss in those with a tendency to lose it, and that its treatment helped maintain bone density and prevent bone loss more than Vitamin D and synthetic estrogen.
An analysis of several studies on the effects of Vitamin K on calcium metabolism suggested that people suffering from osteoporosis are also at a greater risk for stroke and cardiovascular disease, particularly calcification of the middle layer of arteries, resulting in arteriosclerosis.
Requesting an Osteocalcin Test will give patients some indication of their Vitamin K (K2) status, since carboxylation (of osteocalcin) is dependant on Vitamin K2. This in turn will give them some idea of their risk for osteoporosis, and - to some degree - cardiovascular disease.
Stomach acid is another very important aspect with osteoporosis through its implication on calcium and magnesium levels, whereby high acid levels encourage calcium loss, and low levels promote an excessive storage of calcium (calcification, spurs), resulting in bio-unavailability of calcium (see bottom of page). Both extremes - too much or too little stomach acid - have an unfavorable impact on osteoporosis.
Using calcium citrate in low-acid cases, and calcium carbonate in high-acid cases will compensate to some degree, but taking calcium with meals, and supplementing it at smaller amounts (500mg or less at a time) throughout the day will help the absorption of all types of calcium, and somewhat negate the otherwise negative effects of abnormally high or low stomach acid levels (see "Calcium & Magnesium" for additional information on stomach acid interactions, and solubility and absorbability of various types of calcium).
Chromium & Copper also contribute to healthy bones and are effective nutritional remedies that reduce the risk for osteoporosis, however since copper levels are invariably much higher than chromium levels, the high copper / low chromium ratio in practice actually encourages osteoporosis by resulting in a weaker trabecular bone, and frequently arthritis and other inflammatory diseases as well. The same applies when chromium is abnormally low in ratio to potassium, selenium, and/or rarely, vanadium. Chromium is required for proper parathyroid functions, so any chromium antagonists (potassium, selenium, copper, or vanadium,) can contribute to, or encourage bone loss if they are supplemented needlessly, or if their levels remain too high for any other medical or dietary reasons.
Since the consumption of sweets (candy, pastries, sweet fruit, sugar-added foods, pop, honey), as well as alcohol increase chromium requirements, and since these are rarely met with most individuals unless extra amounts are supplemented, Sugar, from refined and natural sources - or all simple carbs - are a major overlooked factor when dealing with osteoporosis, and one that is particularly prevalent in Western Societies. (see also "Sugar & Glycemic Index").
While complex carbohydrates from grain sources do not promote VLDL triglycerides, and are thus much healthier than simple carbs in regard to cardiovascular diseases and other medical conditions, consuming large amounts (of complex carbs) may in some individuals result in a higher phosphorus / calcium ratio, which is also a common cause of osteoporosis.
Strontium is not considered to be an essential trace mineral for humans at this time, however it can now be found in many nutritional formulations, in products that offer nutritional support in the treatment or prevention of bone loss, and some drugs used to treat osteoporosis, such as Protelos (strontium ranelate).[3]
The action of strontium is closely related to that of calcium, although strontium retention varies inversely with calcium intake. Normal diets provide just a few mgs of strontium a day, however to treat or prevent bone loss, over 1,000 mg of strontium has to be ingested daily. This has the potential of causing a large number of side effects, which should be kept in mind when considering the addition of any forms of strontium in the treatment of osteoporosis. (see "Strontium" for additional details and side effects).
Finally, there are those who claim that a high Protein intake is the most common cause of osteoporosis in Western Societies. While high protein intake - particularly from Fad Diets - is definitely a concern not only for osteoporosis, but also kidney functions, it is phosphorus, the end product of protein metabolism that needs to be evaluated. It really doesn't matter whether one deals with abnormally high phosphates from high protein or high grain consumption. Subsequently, high protein intake is safe in regard to bone density and kidney functions as long as an individual's phosphorus status remains normal.
Still, many Vegetarians are under the assumption that in contrast to omnivores, their lower protein intake protects them from osteoporosis, however a high grain intake, or high sugar intake puts them into the same risk as those following a high meat / protein diet.
It should also be mentioned that high oxalic acid-containing food sources such as spinach, rhubarb, beet greens, or chards can have a very negative impact on individuals who have difficulty maintaining adequate levels of calcium. As a result, they are equally at risk to develop osteoporosis since oxalic acid binds to calcium and so reduces its absorption. Kale, broccoli, or collards are a better choice in such cases.
See details and reasons why Coral Calcium and AAACa / AdvaCAL Calcium therapy is not recommended.
High Calcium-related Osteoporosis may develop as a result of
- excessive intake of calcium through dietary or supplemental sources,
- excessive retention of calcium due to genetic disposition,
- low stomach acid, H. Pylori infection, or long-term use of acid-lowering drugs,
- a lack of calcium co-factors (Vitamin C, manganese, phosphorus, magnesium, zinc, omega 3, protein...), which will render calcium bio-unavailable and promote soft tissue calcification, or bone spurs instead.
Unfortunately, many medical doctors and alternative practitioners routinely recommend extra calcium without any tests substantiating their requirements, and subsequently put patients who retain too much calcium at an increased risk for developing cardiovascular disease and joint disorders, including osteoporosis!
In the presence of High Calcium Levels - oxalic acid or phosphorus-rich sources, extra co-factors (above), or any acid-forming foods such as meat, seafood, eggs, dairy, pasta, bread.., would either prevent excessive uptake and storage of calcium, or with the exception of oxalic acid, they would help render calcium more soluble by increasing bioavailability, and subsequently absorption into bone. Increasing stomach acid levels has the same effect, while adequate Vitamin K2 intake prevents calcification of soft tissue through its effect on osteocalcin.

 Manganese may help with some symptoms of Parkinson's disease such as muscle rigidity and twitching...
Manganese may help with some symptoms of Parkinson's disease such as muscle rigidity and twitching...
 Research shows that phytosterols such as beta-sitosterol may help normalize the function of natural killer cells and T-helper lymphocytes...
Research shows that phytosterols such as beta-sitosterol may help normalize the function of natural killer cells and T-helper lymphocytes...
 Iron deficiency may be suspect with some forms of ADHD. 84% of children with ADHD were found to have abnormally low levels of ferritin...
Iron deficiency may be suspect with some forms of ADHD. 84% of children with ADHD were found to have abnormally low levels of ferritin...
 A high intake of B Vitamins can trigger heart palpitations, HBP, major complications in patients with congestive heart disease...
A high intake of B Vitamins can trigger heart palpitations, HBP, major complications in patients with congestive heart disease...